Featured
HIV/AIDS: The odds against SDGs 2030 ambition
Published
10 years agoon
By
Olu Emmanuel
Although clinically viable vaccine is beginning to reboot hope of halting deaths arising from HIV infections around the world pretty soon, spiraling incidence of new infections may, however, be a clog in eliminating the pandemic as envisioned in the.
By GBENGA OGUNDARE
EXPERTS say AIDS deaths are plummeting fast in most countries around the world, but that’s not exactly a cheery news yet. Another dizzying truth is that the rate of new infections, according to the Institute for Health Metrics and Evaluation [IHME] has equally spiralled in several countries over the past decade, thus threatening ambition to end the AIDS scourge by 2030.
A study from the Global Burden of Disease collaborative network found that 74 countries saw increases in age-standardized rates of new infections between 2005 and 2015, including South-Africa, Egypt, Pakistan, Kenya, the Philippines, Cambodia, Mexico, and Russia.
The new research, released at the International AIDS Conference in Durban, South Africa July 2016, also found that while the global number of new cases continues to decline, the pace has greatly slowed. New infections of HIV fell by an average of only 0.7 percent per year between 2005 and 2015—compared to the 2.7 percent drop per year between 1997 and 2005.
“If this trend of stubbornly high new infections continues, there will be significant challenges in meeting the UN’s Sustainable Development Goal for the world to witness the end of AIDS in less than 15 years,” said IHME Director, Dr. Christopher Murray.
“Everyone in population health — researchers, policymakers, practitioners, pharmaceutical companies, advocates, and others — needs to understand that even if more people are living with HIV, we cannot end AIDS without stopping new infections.”
That’s no doomsaying from Murray really. Rather, Professor Peter Piot, founding executive director of UNAIDS, thinks it’s merely being brutally frank. “This study shows that the AIDS epidemic is not over by any means and that HIV/AIDS remains one of the biggest public health threats of our time.”
“The continuing high rate of over 2 million new HIV infections represents a collective failure which must be addressed through intensified prevention efforts and continued investment in HIV vaccine research.”
The study examines HIV mortality, prevalence, and incidence between 1980 and 2015, and is part of the Global Burden of Disease Study 2015, which provides comprehensive population health estimates on disease, injuries, and related risk factors.
In contrast to the overall slow decline in new infections, the number of people living with HIV has significantly increased globally, largely due to the expansion of antiretroviral therapy (ART). IHME estimates there were about 39 million people globally living with HIV in 2015, as compared to 28 million in 2000.
In 2015, 41 percent of the people living with HIV were using ART, as compared to less than 2 percent in 2000.
“We’re keeping people alive longer, and these numbers should give those using antiretroviral therapies considerable hope,” said IHME Associate Professor Dr. Haidong Wang, the lead author on the study.
But the improvement remains marginal—far away from the ambitious 90-90-90 goals set by the global community for the year 2020. Those goals aim for 90% of people living with HIV knowing their HIV status, 90% of people diagnosed with HIV receiving antiretroviral therapy, and 90% of people receiving antiretroviral therapy experiencing viral suppression.
Instructively, there is a striking difference in the use of ART between men and women. On average, global ART use is 10 percent higher among women living with HIV, and in some sub-Saharan nations in 2015, it is 50 percent higher. However, in some Eastern European and South Asian nations, the percentage of men using ART is as much as 50 percent higher than women.
“The Global Burden of Disease HIV study provides critical health information to help shape and support national and global decision-making,” said Peter Hayward, editor of The Lancet HIV. “The estimates are also key to strengthening accountability to ensure that promises made by politicians and policymakers with regard to specific HIV targets are being delivered.”
A dint of hope
Funding for HIV/AIDS advocacy campaigns around the world have apparently plunged over the years, but maybe not exactly so with research efforts to find a permanent panacea. And that tenacity is rebooting hope of an HIV-free generation already.
Result from a new study by a team of AIDS scientists is leading the way to the development of an effective human vaccine against the human immunodeficiency virus (HIV).
In the study, researchers worked with a species of Old World monkeys, Rhesus Macaques, to reproduce the trial results of RV144, the only HIV vaccine that has been tested and shown to reduce the rate of HIV acquisition in a phase III clinical trial.
Researchers were interested in not only recapitulating the findings from the RV144 trial, but also determining if replacing the alum adjuvant–a substance commonly found in non-living vaccines known to induce antibody-mediated immunity–with a different adjuvant, MF59 would decrease simian immunodeficiency virus (SIV) acquisition at an increased rate and yield a more efficacious vaccine.
Although MF59 is known to help stimulate the human body’s immune response, the idea that it could lead to greater vaccine efficacy is a popular working theory shared by scientists worldwide.
Rafick-Pierre Sekaly, the Richard J. Fasenmyer Professor of Immunopathogensis helped to lead the study which simulated potential HIV infection by rectally challenging the macaques with SIV, the primate form of HIV. Simulation in macaques has been a critical step in progressing HIV research, since the virus does not replicate well in most other model organisms.
ALSO SEE: 700,000 Nigerian adolescent are HIV/AIDS positive – UNICEF
With this simulation complete, researchers were able to successfully reproduce the RV144 trial results in macaques, ultimately finding that the RV144 vaccine combined with the alum adjuvant reduced the risk of acquisition by 44 percent, which is within the range of the 31 percent efficacy previously measured in humans.
However, researchers were surprised to learn that changing the adjuvant to MF59 did not result in a significantly better vaccine, but instead rendered the altered vaccine unable to prevent SIV acquisition at a greater rate and triggered an adaptive immune response only at the site of infection, thereby disproving the commonly believed hypothesis.
Importantly, researchers were able to uncover more about the alum group’s mode of action in the RV144 vaccine which, to-date, is not fully understood.
Researchers discovered a unique association between an intercellular pathway known as Ras-Raf-MEK-ERK (RAS) and the efficacy of RV144. Ten of twelve genes associated with the RAS pathway were expresses within the vaccine and have been shown to trigger several subsets of innate and adaptive responses that, in turn, are associated with a decreased risk of SIV acquisition in the alum-vaccine group. Whether RAS activation is an important hallmark of HIV-vaccine efficacy in humans is an area for further study.
According to Dr. Sekaly, “These fascinating clinical results effectively dispel our previous belief that the RV144 vaccine could possibly become more effective with the MF59 adjuvant. Instead, we found that the modified vaccine actually triggered the recruitment of innate cells in the site of infection. Through this research, we were able to confirm the efficacy of the current RV144 vaccine in preventing infection by HIV/SIV in macaques, creating an even clearer pathway to the near-term development of this vaccine for human use.”
Based on the pre-vaccination RNA expression of the macaque, Dr. Sekaly and his team were also able to accurately predict whether or not the animal was going to respond to the RV144 vaccine in alum, correctly forecasting the response in two thirds of the macaques tested. These findings have tremendous implications for the use of personalized medicine in vaccinology, an exciting exploration of genomics that is already underway in the scientific community.
ALSO SEE: Only change of behavior can stem HIV/AIDS scourge, institute declares
“We have seen that pre-selecting subjects that will benefit from a therapy based on their predicted response or risk of disease is an excellent way to improve potential outcomes,” said Dr. Sekaly. “These study results strongly support the notion that personalized and predictive vaccinology will soon become a reality, including in HIV–a disease area for which this type of precision medicine is desperately needed but has not yet been extensively studied.”
Approximately 1.2 million people died from HIV in 2015, down from a peak of 1.8 million in 2005. And in regard to mortality, study shows that women tend to die at younger ages from the disease than men—likely due to age-disparate relationships in which men have sex with younger women.
Not for the fun of it. The results of the IHME’s study underscores the need for more effective efforts to prevent new infections, as well as additional funding for this drive.
Yet analysis shows that development assistance for health (DAH) targeting HIV/AIDS grew fastest between 2000 and 2009, yet such funding has stagnated since 2010.
According to Financing Global Health 2015, a report published in April by IHME, annual funding globally for HIV/AIDS peaked at US$11.2 billion in 2013, but dropped to US$10.8 billion in 2015—a reality that presents the world with two unpleasant consequences.
For sure, sustained slowdown in the decline of new infections and in funding for HIV/AIDS, can only frustrate the ambition by the global community to end AIDS by 2030.
You may like

NOA Director General Lanre Issa-Onilu supports tax reform to improve Nigerians’ lives


House of Reps member Dogonyaro is dead


Oyo Govt vows to achieve 100% literacy level
Nigeria’s $100B SDG financing deal: Fantasy or reality?
Director in N30m HIV/AIDS funds scandal
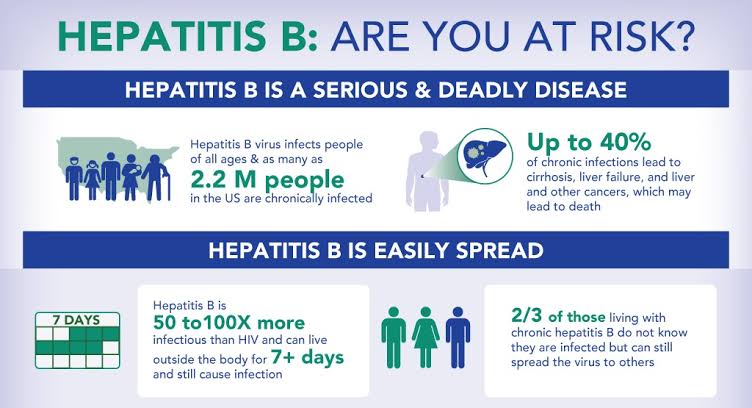
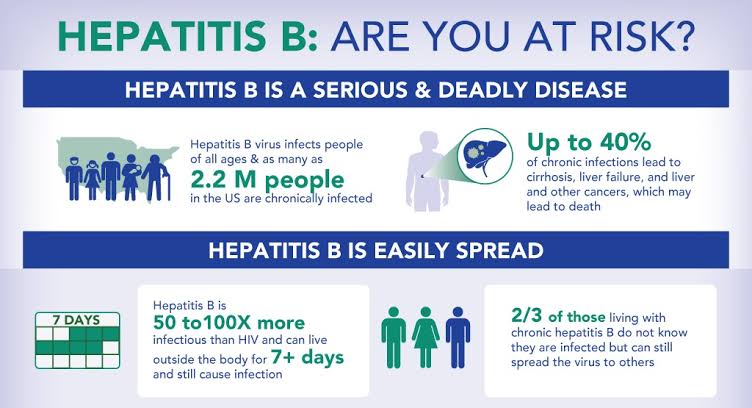
Why Hepatitis B may be more dangerous than HIV, says expert
Trending
 Health5 days ago
Health5 days agoDeclassified CIA memo explored concealing mind-control drugs in vaccines

 Entertainment7 days ago
Entertainment7 days agoSimi addresses resurfaced 2012 tweets amid online backlash

 Crime6 days ago
Crime6 days agoSenior police officers faces retirement after Disu’s appointment as acting IGP

 Education1 week ago
Education1 week agoPeter Obi urges JAMB to address registration challenges ahead of exams

 Health1 week ago
Health1 week agoNAFDAC issues alert on suspected revalidated SMA Gold infant formula

 Comments and Issues6 days ago
Comments and Issues6 days ago20 Critical Fixes to Save Nigeria’s Democracy from Electoral Fraud

 Football7 days ago
Football7 days agoMartínez ruled out of Everton clash with calf injury

 Latest6 days ago
Latest6 days agoICPC yet to respond to El-Rufai’s bail request as arraignment date looms

